There has been no convincing evidence of cause-effect relationships between radiation exposures from the Chernobyl accident (CA) and the incidence increase of cancers in residents of contaminated territories except for thyroid cancer (TC) in people exposed at a young age [1]; therefore, pediatric TC is predominantly discussed here below. Since 2009 we have defended the hypothesis [2–7] that the registered increase in the TC incidence after CA was largely caused by the screening, improved medical surveillance and registration of unexposed patients as exposed. The “successive waves of tumors in those exposed to high levels of fallout as children, each with different molecular, morphological, and clinical findings” [8] after CA were largely determined by changing intensity of the screening, improving accuracy of diagnostics and registration, exhaustion by the screening of the pool of neglected cancers [2–7]. TC had been under-diagnosed and under-reported before CA. The incidence of TC among people younger than 15 years in the “five most northerly regions” of Ukraine was 0.1 and in Belarus — 0.3 cases/million/year from 1981 through 1985 [9]. Worldwide, the incidence of TC in children was estimated at 0.5–1.2 and in adolescents — 4.4–11 cases/million/year [10]. The figures tend to be higher in more developed countries [10,11] obviously due to better diagnostics. Many experts argue that the gradual increase in TC incidence worldwide is caused by technological advancements in diagnostics. At the same time, the long-term mortality from differentiated TCs declined or stabilized almost everywhere [10]. Only 5 children were diagnosed with TC in Belarus in the period 1978–1985, the detection rate of pediatric TC prior to CA being much lower than that in other developed countries [11]. This indicates that there were undiagnosed cases in the population. Some neglected advanced cancers, detected by the screening, self-reported in conditions of increased public awareness after CA, or brought from other areas and registered as Chernobyl victims, were misinterpreted as rapidly growing radiogenic malignancies [2–7]. Many people strived for the registration as Chernobyl victims to gain access to health care provisions [12]. Cases from non-contaminated areas must have been averagely more advanced as there was no extensive screening there. The proposed increase in the “aggressivity” of cancers after the radioactive contamination in the Chernobyl area [13] apparently resulted from detection by the screening of old neglected malignancies, interpreted as radiogenic tumors with the “rapid onset and aggressive development” [13].
International comparisons are informative in this connection. Differences in the average histological grade of malignancies may reflect the diagnostic quality and averagely earlier or later tumor detection in a given country. This hypothesis has been supported by comparisons of renal cancer (RC) specimens from Ukraine with random cases from Colombia and Spain. RCs from Ukraine were averagely less differentiated than the overseas counterparts [14–20]. The differences can be attributed to a more efficient and early cancer diagnostics in Spain and Colombia [21]. The proposed increase in the “aggressivity” of RC and TC after the radioactive contamination in the Chernobyl area apparently resulted from detection by the screening of old neglected cases, interpreted as radiogenic tumors with the “rapid onset and aggressive development” [13]. The screening detected not only small nodules but also advanced tumors, neglected because of the incomplete coverage of the population by medical checkups. This is confirmed by the fact that the “first wave” TCs (found during ~10 years following CA) were on average larger and higher-grade than those diagnosed later [22].
Some molecular-genetic markers of RC from Ukraine vs. those from Spain and Colombia need a re-interpretation. The marker VEGF was found more frequently in clear-cell renal cell carcinoma from Ukraine [20]. The “level of serum VEGF has been shown to be closely related to tumor stage and grade of renal cell carcinoma, and the expression of VEGF to be significantly associated with tumor stage” [20]. Other studies also reported associations between VEGF and microvascular density, stage and grade of RC. The same considerations probably apply to other markers, where differences between the Spanish and Ukrainian RCs were found, in particular, NF-kappa-B, its p50 and p65 subunits [17]. The >10 % cell positivity for p50 was found in 25 from 59 (42.4 %) of specimens from Ukrainian vs. 4 from 19 (21.1 %) of Spanish patients; the >50 % p65 positivity was found, correspondingly, in 18 from 59 (30.1 %) vs. 1 from 19 (5.3 %) of the specimens (p<0.05) [17]. In accordance with the concept presented here, NF-kappa-B activation has been discussed in the literature as a marker and promoter of the neoplastic progression.
The analogy with RET/PTC3 chromosomal rearrangements in papillary thyroid carcinoma (PTC) is further helpful. According to our hypothesis, the frequency of RET/PTC3 positivity in PTC specimens correlates with the average tumor grade and hence with the disease duration [4,6]. This is not surprising as mutations generally tend to accumulate with the neoplastic progression. For example, mutations were found in TCs from Russia more frequently than in those from the United States [23,24], which indicates earlier diagnostics in the latter country. An association was found between RET/PTC3 and aggressive phenotype, advanced stage and larger size of PTC [25]. With the time passing after CA, the prevalence of RET/PTC3 in Chernobyl-related TCs declined [8,26,27] while advanced neglected tumors were sorted out by the screening. The cohort of post-Chernobyl pediatric PTCs, with RET/PTC3 as a prevailing RET rearrangement type, was supposed to be worldwide exceptional [28]. In fact, this cohort is exceptional not worldwide but for industrialized high-income countries where cancer is diagnosed relatively early. Similarly to Chernobyl, RET/PTC3 was the most prevalent RET rearrangement in the studies from India [29,30]. Asian populations generally demonstrated a higher positivity rate for RET/PTC3 than Western populations (26.50 % vs. 17.05 %) [31] with the exception of such highly developed country as Japan (discussed below). Along the same lines, RET/PTC3 are rare in France [32], which suggests an averagely early tumor detection.
The comparison between the former Soviet Union (SU) and Japan is not straightforward because screening activities after the Chernobyl and Fukushima Daiichi accidents have been confounding factors. Obviously, CA had a greater impact on the diagnostic practices in the former SU than the Fukushima accident in Japan. The registered TC incidence in Belarus in people ≤18 years old has remained at an enhanced level — several times higher than in Western countries [27], although the radiation factor has no longer been active and no country-wide screening was performed [27], which indicates that other mechanisms e. g. enhanced vigilance and over-diagnosis have contributed to the high detection rate. In accordance with the concept discussed here, the frequency of RET/PTC3 in Japan is relatively low [31,33]. Japanese pediatric TCs have been different from those in Belarus and Ukraine, showing less frequently the de-differentiated solid and solid-trabecular patterns [34,35]. Unlike Chernobyl, most TCs after the Fukushima accident were of the classical papillary type i. e. having a comparatively high differentiation grade [36,37]. International comparisons of the TC grade may be more informative than those of the stage because large nodules with uncertain malignant potential can be classified as high-stage cancers if there is a propensity to histo- and cytological over-diagnosis in conditions of hypervigilance, insufficient quality of specimens and disagreements between panel members [2,6,38,39]. The hypervigilance can be illustrated by the following citation: “Practically all nodular thyroid lesions, independently of their size, were regarded at that time in children as potentially malignant tumors, requiring an urgent surgical operation” [40]. Potential mechanisms of the over-diagnosis have been discussed previously [2,6].
The misclassification of advanced cases as aggressive radiogenic cancers has given rise to the concept that radiogenic TCs are more aggressive than sporadic ones [13,41]. This had consequences for the practice: the surgical treatment of radiogenic TC was recommended to be more radical [42]. In the 1990s, the thyroid surgery in some institutions of the former SU adopted more radical methods; details and references are in [7,43]. Reasonable considerations about TC over-diagnosis and overtreatment can be found in the recent review: “After the Chernobyl and Fukushima nuclear accidents, thyroid cancer screening was implemented mainly for children, leading to case over-diagnosis;” “The existence of a natural reservoir of latent thyroid carcinomas, together with advancements in diagnostic practices leading to case over-diagnosis explain, at least partially, the rise in TC incidence in many countries;” “Total thyroidectomy, as performed after the Chernobyl accident, implies patients must live the rest of their lives with thyroid hormone supplementation. Additional treatment using radioactive iodine-131 therapy in some cases may result in potentially short- or long-term adverse effects” [44]. Preceding publications expressing the same concept [2–6,43] have not been cited in [44]. Obfuscation of the over-diagnosis and overtreatment of post-Chernobyl TCs and other lesions is recognizable in the literature from the former SU. Certain authors know our publications on this topic [2–7,43,45] but do not cite them in spite of personal communications. In the earlier report with participation of Prof. E. Dillwyn Williams (2008) it was stated that “The exposed and unexposed tumors from the same geographical area are essentially identical morphologically and in their degree of aggressiveness… childhood PTCs from Japan were much more highly differentiated (p<0.001), showed more papillary differentiation (p<0.001) and were less invasive (p<0.01) than ‘Chernobyl’ tumors” [34]. Later on, in unsupervised publications by the co-authors, the accents were changed, e.g.: “Childhood Japanese PTCs differed from Ukrainian PTCs by more pronounced invasive properties… higher morphological aggressiveness of PTC in young Japanese patients” [35]. In last paper by the same researchers it was acknowledged that Ukrainian “radiogenic” or “radiation-related” PTCs “had a solid-trabecular growth pattern and displayed morphological features of aggressive biological behavior” [41] without any satisfactory proof that (a considerable part of) tumors in the studied residents of Kiev, Chernigov and Zhitomir provinces [41] were caused or influenced by radiation. What was indeed different about inhabitants of these regions were the screening with detection of neglected cases and some over-diagnosis, radiophobia with increased self-reporting, as well as registration of some unexposed people as Chernobyl victims [6,7,12]. The cases coming from non-contaminated areas must have been averagely more advanced as there was no mass screening there. We intended to comment on the article [41] by a letter to the editor but it was possible only against payment (fig. 1), which is an obstacle for a scientific discussion. Therefore this commentary is published here.
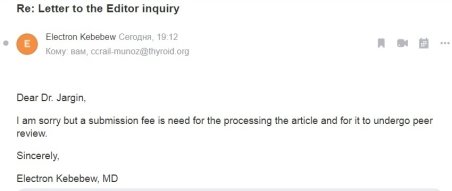
Fig. 1. The message that a “fee is need for the processing the article and for it to undergo peer review” for a letter to the editor commenting on [41], signed by Electron Kebebew
In conclusion, international differences in the histological grade of malignancies may reflect diagnostic quality, that is, averagely earlier or later tumour detection in a given country. Associations of various markers with the tumor progression (disease duration, tumor grade and stage) is a potential field for the future research and re-interpretation of the data already obtained in studies comparing malignancies from different regions. Some markers may characterize an averagely later or earlier cancer detection in a given country and hence the efficiency of healthcare services.
References:
- UNSCEAR 2008 Report to the General Assembly. Annex D. Health effects due to radiation from the Chernobyl accident. New York: United Nations, 2008.
- Jargin SV. Thyroid carcinoma in children and adolescents resulting from the Chernobyl accident: possible causes of the incidence increase overestimation. Cesk Patol 2009;45:50–52.
- Jargin SV. Thyroid cancer after Chernobyl: obfuscated truth. Dose Response 2011;9:471–6.
- Jargin SV. RET/PTC3 rearrangement in papillary thyroid carcinoma: possible marker of tumor progression. Ann Surg 2017;266:e120–1.
- Jargin SV. Hormesis and radiation safety norms: Comments for an update. Hum Exp Toxicol 2018;37:1233–43.
- Jargin SV. The overestimation of medical consequences of low — dose exposure to ionizing radiation. Newcastle upon Tyne: Cambridge Scholars Publishing, 2019.
- Jargin SV. Markers of radiogenic cancer vs. tumor progression: an overview of Chernobyl studies. J Cancer Sci 2021;8:7.
- Williams D. Radiation carcinogenesis: lessons from Chernobyl. Oncogene 2008;27 Suppl 2:S9–18.
- Stsjazhko VA, Tsyb AF, Tronko ND, et al. Childhood thyroid cancer since accident at Chernobyl. BMJ 1995;310:801.
- Drozd V, Saenko V, Branovan DI, et al. A search for causes of rising incidence of differentiated thyroid cancer in children and adolescents after Chernobyl and Fukushima: comparison of the clinical features and their relevance for treatment and prognosis. Int J Environ Res Public Health 2021;18:3444.
- Demidchik YE, Saenko VA, Yamashita S. Childhood thyroid cancer in Belarus, Russia, and Ukraine after Chernobyl and at present. Arq Bras Endocrinol Metabol 2007;51:748–62.
- Bay IA, Oughton DH. Social and economic effects. In: Smith J, Beresford NA (eds) Chernobyl — catastrophe and consequences. Chichester: Springer, 2005; pp 239–66.
- Yablokov AV, Nesterenko VB, Nesterenko AV. Consequences of the Chernobyl catastrophe for public health and the environment 23 years later. Ann N Y Acad Sci 2009;1181:318–26.
- Romanenko A, Morell-Quadreny L, Nepomnyaschy V, Vozianov A, et al. Pathology and proliferative activity of renal-cell carcinomas (RCCS) and renal oncocytomas in patients with different radiation exposure after the Chernobyl accident in Ukraine. Int J Cancer 2000;87:880–3.
- Romanenko A, Morell-Quadreny L, Nepomnyaschy V, et al. Radiation sclerosing proliferative atypical nephropathy of peritumoral tissue of renal-cell carcinomas after the Chernobyl accident in Ukraine. Virchows Arch 2001;438:146–53.
- Romanenko A, Morell-Quadreny L, Ramos D, et al. Extracellular matrix alterations in conventional renal cell carcinomas by tissue microarray profiling influenced by the persistent, long-term, low-dose ionizing radiation exposure in humans. Virchows Arch 2006;448:584–90.
- Romanenko A, Morell-Quadreny L, Ramos D, et al. Alteration of apoptotic regulatory molecules in conventional renal cell carcinoma influenced by chronic long-term low-dose ionizing radiation exposure in humans revealed by tissue microarray. Cancer Genomics Proteomics 2006;3:107–12.
- Morell-Quadreny L, Romanenko A, Lopez-Guerrero JA, et al. Alterations of ubiquitylation and sumoylation in conventional renal cell carcinomas after the Chernobyl accident: a comparison with Spanish cases. Virchows Arch 2011;459:307–13.
- Romanenko AM, Ruiz-Saurí A, Morell-Quadreny L, et al. Microvessel density is high in clear-cell renal cell carcinomas of Ukrainian patients exposed to chronic persistent low-dose ionizing radiation after the Chernobyl accident. Virchows Arch 2012;460:611–9.
- Ruiz-Saurí A, Valencia-Villa G, Romanenko A, et al. Influence of exposure to chronic persistent low-dose ionizing radiation on the tumor biology of clear-cell renal-cell carcinoma. An immunohistochemical and morphometric study of angiogenesis and vascular related factors. Pathol Oncol Res 2016;22:807–15.
- Jargin SV. Renal cell carcinoma after Chernobyl: on the role of radiation vs. late detection Pathol Oncol Res 2015;21:845–946.
- Williams ED, Abrosimov A, Bogdanova T, Demidchik EP, Ito M, LiVolsi V, et al. Thyroid carcinoma after Chernobyl latent period, morphology and aggressiveness. Br J Cancer 2004;90:2219–24.
- Kimmel RR, Zhao LP, Nguyen D, et al. Microarray comparative genomic hybridization reveals genome-wide patterns of DNA gains and losses in post-Chernobyl thyroid cancer. Radiat Res 2006;166:519–31.
- Troshin VP. Characteristic of thyroid cancers in the region suffered after accident at the Chernobyl nuclear power plant (years 1986–2006). Dissertation. St. Petersburg: 1st Medical University, 2009.
- Romei C, Elisei R. RET/PTC translocations and clinico-pathological features in human papillary thyroid carcinoma. Front Endocrinol 2012;3:54.
- Rabes HM, Demidchik EP, Sidorow JD, et al. Pattern of radiation-induced RET and NTRK1 rearrangements in 191 post-Chernobyl papillary thyroid carcinomas: biological, phenotypic, and clinical implications. Clin Cancer Res 2000;6:1093–103.
- Rogounovitch TI, Mankovskaya SV, Fridman MV, et al. Major oncogenic drivers and their clinicopathological correlations in sporadic childhood papillary thyroid carcinoma in Belarus. Cancers (Basel) 2021;13:3374.
- Nikiforov YE. Molecular diagnostics of thyroid tumors. Arch Pathol Lab Med 2011;135:569–77.
- Khan MS, Qadri Q, Makhdoomi MJ, et al. RET/PTC gene rearrangements in thyroid carcinogenesis: assessment and clinico-pathological correlations. Pathol Oncol Res 2020;26:507–13.
- Rao PJ, Vardhini NV, Parvathi MV, et al. Prevalence of RET/PTC1 and RET/PTC3 gene rearrangements in Chennai population and its correlation with clinical parameters. Tumor Biol 2014;35:9539–48.
- Su X, Li Z, He C, et al. Radiation exposure, young age, and female gender are associated with high prevalence of RET/PTC1 and RET/PTC3 in papillary thyroid cancer: a meta-analysis. Oncotarget 2016;7:16716–30.
- Bounacer A, Wicker R, Caillou B, et al. High prevalence of activating ret proto-oncogene rearrangements, in thyroid tumors from patients who had received external radiation. Oncogene 1997;15:1263–73.
- Vuong HG, Altibi AM, Abdelhamid AH, et al. The changing characteristics and molecular profiles of papillary thyroid carcinoma over time: a systematic review. Oncotarget 2017;8:10637–49.
- Williams ED, Abrosimov A, Bogdanova T, et al. Morphologic characteristics of Chernobyl-related childhood papillary thyroid carcinomas are independent of radiation exposure but vary with iodine intake. Thyroid 2008;18:847–52.
- Bogdanova TI, Saenko VA, Hirokawa M, et al. Comparative histopathological analysis of sporadic pediatric papillary thyroid carcinoma from Japan and Ukraine. Endocr J 2017;64:977–93.
- Suzuki S. Childhood and adolescent thyroid cancer in Fukushima after the Fukushima Daiichi nuclear power plant accident: 5 years on. Clin Oncol (R Coll Radiol) 2016;28:263–71.
- Yamashita S, Suzuki S, Suzuki S, et al. Lessons from Fukushima: latest findings of thyroid cancer after the Fukushima Nuclear Power Plant accident. Thyroid 2018;28:11–22.
- Bogdanova TI, Zurnadzhy LY, Greenebaum E, et al. A cohort study of thyroid cancer and other thyroid diseases after the Chornobyl accident: pathology analysis of thyroid cancer cases in Ukraine detected during the first screening (1998–2000). Cancer 2006;107:2559–66.
- LiVolsi VA, Abrosimov AA, Bogdanova T, et al. The Chernobyl thyroid cancer experience: pathology. Clin Oncol (R Coll Radiol) 2011;23:261–7.
- Lushnikov EF, Tsyb AF, Yamashita S. Thyroid cancer in Russia after the Chernobyl. Moscow: Meditsina, 2006.
- Bogdanova TI, Saenko VA, Hashimoto Y, et al. Papillary thyroid carcinoma in Ukraine after Chernobyl and in japan after Fukushima: different histopathological scenarios. Thyroid 2020; DOI: 10.1089/thy.2020.0308.
- Rumiantsev PO. Thyroid cancer: modern approaches to diagnostics and treatment. Moscow: Geotar-Media, 2009.
- Jargin SV. Thyroid neoplasia after Chernobyl: a comment. Int J Cancer 2019;144:2897.
- Cléro E, Ostroumova E, Demoury C, et al. Lessons learned from Chernobyl and Fukushima on thyroid cancer screening and recommendations in case of a future nuclear accident. Environ Int 2021;146:106230.
- Jargin SV. Urological concern after nuclear accidents. Urol Ann 2018;10:240–2.