To establish the remoteness of death changes of leukocytes the amount of T- and B-lymphocytes were analyzed in dynamics by the method of rosetting with erythrocytic CD3, CD4, CD8, CD25, CD22 diagnostic sets, and NO concentration in plasma was determined, as well. Disturbances of changes in the amount of T- and B-lymphocytes expressing molecules-markers CD3, CD4, CD8, CD25, CD22. Dramatic elevation of NO concentration in plasma was observed in 2–6 hours time interval. Further the decrease of NO concentration was recorded in 7–16 hours time interval in case of deaths due to CHD and in the time interval 12–21 hours in case of deaths due to mechanical traumas. The detected changes of immune indices and NO concentration in plasma may be used to establish the remoteness of death in medicolegal practice.
Keywords: time since of death, T-and B-lymphocytes, expression of molecules CD3, CD4, CD8, CD22, CD25, level of nitrates/nitrites.
С целью установления давности наступления смерти (ДНС) определяли в динамике количество Т- и В-лимфоцитов методом розеткообразования с эритроцитарными CD3, CD4, CD8, CD22, CD25-диагностикумами и концентрации NO в плазме. Выявлены изменения количества Т- и В-лимфоцитов, экспрессирующих молекулы-маркёры CD3, CD4, CD8, CD22, CD25. В период времени 2–6 часов наблюдалось увеличение концентрации NO. В дальнейшем отмечалось снижение концентрации NO при ишемической болезни сердца (ИБС) в промежутке времени от 7 до 16 часов, а при смерти от механических травм — от 12 до 21 часа. Обнаруженные изменения иммунных показателей и концентрации NO в плазме могут быть использованы в судебно-медицинской практике для установления ДНС.
Ключевые слова: давность наступления смерти, Т-, В-лимфоциты, экспрессия молекул CD3, CD4, CD8, CD22, CD25, уровень нитратов/нитритов.
The problem of diagnosis of Time of Death (TOD) has been developed for a century and a half by many scientists around the world. One of the main directions in the development of this problem is the research of postmortem phenomena flowing in organs, tissues and liquids [1, 2, 3, 4, 5].
The results indicated the need for a more in-depth study of the facility based on immunological methods. Immunological tests were used based on the evaluation of the survival properties of the lymphocytes involved in the immune response of the body to the injury, disease, and the use of information on the time of exposure to the body. Researchers have found that neutrophils are rapidly degraded in the blood in the postmortem period and when blood is stored in vials, while blood lymphocytes retain a significantly longer life span [6].
In recent years, in order to address the issue of the TOD, forensic science and practice have started by seeking new directions involving the use of more objective laboratory methods of research. The possibility of using the blast transformation reaction, T- and B-lymphocyte outlet formation and the quantitative content of immunoglobulin to determine the TOD, as well as the timing of the suitability of the blood to diagnose the TOD when stored under different conditions [7].
Levels of impaired immune status, cellular metabolism and morphogenesis in sudden cardiac death, alcoholic cardiomyopathy, acute myocardial infarction have been established relatively recently. Peculiarities of cytokine balance at sudden cardiac death have been studied, described and analyzed. The algorithm of differential diagnostics, alcoholic cardiomyopathy and atherosclerotic heart disease based on a complex of immunological and biochemical indicators is offered [8].
There are sporadic reports in the literature on the role of nitrates/nitrites in determining the age of damage. For example [8], researchers have found that in myocardium, in the first 3 hours after injury, the amount of induced NO synthase changed little. After 12 hours, there was a sharp decrease in the activity of this enzyme.
Involvement of nitro-producing nitrogen (nitrate and nitrite derivatives) in many pathological processes has been established [9]. The important modulating role of NO in stress reaction is shown, which are many severe neurological (craniocerebral trauma, acute cerebrovascular disorders, especially acute cerebral ischemia) and somatic diseases (sepsis, shock, polytrauma). The stress reaction of the immune neuroendocrine system is triggered by the activation of the main stress-producing axes — the hypothalamo-pituitary-adrenal and sympatho-adrenal axes. The stress reaction, which was primarily adaptive, soon begins to take part in the mechanisms of the pathological process: excessive hormonal changes cause a complex of circulatory and metabolic disorders and close vicious circles of pathogenesis of a disease [10].
The work [8] describes 19 cases of patients dying in hospital from septic shock, in which apoptosis of neurons and cells of the brain microglia, as well as an increase in the level of inducible NO-synthase and the factor of tumor necrosis.
It has been noted that NO can act as a trigger for the initiation of kinase decay of the main regulatory system controlling the expression of a number of genes responsible for the development of apoptosis of cells [11]. Based on the immunohistochemical study of changes in the quantity of NO-synthase in the myocardium, the forensic medical criteria of the limitation of the formation of damage due to mechanical injury are determined.
It should be noted that the literature lacks information on the relationship of the TOD, indicators of cellular and humoral immunity, and nitrate/nitrite levels.
The purpose of our research was to study the amount of T- and B-lymphocytes expressing molecules — markers CD3, CD4, CD8, CD25, CD22 and the level of nitrate/nitrite in plasma depending on the TOD.
Research Materials and Methods
The expression changes of CD22 B cells, CD3, CD4, CD8, CD25 T cells have been determined by means of a socket matching method with appropriate erythrocytic diagnostics [12]. The percentage of rosette-forming lymphocytes in normal light microscopy was calculated, which clearly had at least 3 attached erythrocytes to diagnostics with anti-CD monoclonal antibodies [13].
Nitrite/nitrate levels were determined in the blood plasma by a technique based on the reduction of nitrate to nitrite by zinc dust in an alkaline medium in the presence of an ammonium complex of copper sulfate followed by photometry [11]. Blood plasma from human corpses was taken in dynamics, 2–6, 7–11, 12–16 and 17–21 hours after death. The blood plasma taken from the right heart and large vessels in the corpses of people who died from multiple injuries (20) and from MYOCARIDAL ISCHEMIA (17) were examined. For the purpose of deprotenization, plasma added 1 ml of 6 % zinc sulfate solution to 1 ml. Left for 1 hour at a temperature below 150C. Centrifuged at 6,000 rev/min. After deprotenization, an equivalent amount of sodium hydroxide was added to 1 ml of the supernatant. Then again, centrifuge was carried out and 1 ml of the field fluid was transferred to a numbered plastic vial with 0.11 g of zinc dust, 0.5 ml of ammonia buffer, 20 µl of ammonium sulfate complex of copper. The vials were then shaken for 30 minutes. Zinc dust was centrifuged at 3,000 rev/min — 10 minutes. From each plastic vial, 1 ml of supernatant was carried into a glass vial corresponding to the numbering.
Each vial had 1 ml of sulfanyl acid added and kept in the refrigerator for 10 minutes until the diazonating reaction was complete. Then, 1 ml of sodium acetate solution and 1 ml of 1-naphthylamine saline solution were applied to each vial. The optical density was measured 30 minutes later at 520 nm. The concentration of nitrites/nitrates was calculated according to the calibration schedule, taking into account dilution at deprotenization.
Statistical data processing was carried out with the help of the program Pimer of Biostatistics. Since the distribution of the values studied differed from the normal one, the median of 25 and 75 was used for descriptive statistical analysis. The Wilcoxon-Mann-Whitney criterion [12] was used to compare the differences between groups. The differences were statistically valid at p<0.05.
Results and discussion
The blood of the deceased (n=20) was studied in dynamics from other causes: mechanical injuries (closed TBIs, falls from height) and mechanical asphyxia as a result of hanging. The time interval from 7 to 16 hours was compared with the control group of donors, and the remaining T-cell counts were compared with the results of previous CSN intervals.
A reliable decrease in lymphocytes (p<0.001) expressing the CD3 molecule was noted after death in intervals of 7–16 hours 52 % to 51–64 hours 29 % [48.55; 43.50; 35.43; 31.39; 24.33]. A less reliable decrease in the index (p<0.05) was obtained in the interval from 65 to 78 hours 23 % [21.28] (table 1).
Table 1
T-lymphocytes expressing molecules CD3, CD4, CD8, CD25, CD22 (%) in persons (n=30) who died from other causes of death (mechanical injuries and asphyxiation by hanging)
|
Rate |
CG (n=15) |
Time of death. (TOD) |
|||||
|
7–16 |
17–26 |
27–36 |
37–50 |
51–64 |
65–78 |
||
|
СD3 |
58,1(55,0–59,1) |
52,0(48,0–55,0)*** |
46,0(43,0–50,0)*** |
42,0(35,0–43,0)*** |
36,0(31,0–39,0)*** |
29,0(24,0–33,0)*** |
23,0(21,0–28,0)* |
|
CD4 |
42(40,3–53,5) |
36,0(31,0–38,0)*** |
30,5(25,0–35,0)*** |
28,0(22,0–30,0)* |
24,0(20,0–27,0)** |
18,0(17,0–20,0)*** |
14,0(12,0–16,0)*** |
|
CD8 |
22,6(21,5–24,0) |
18,0(17,0–19)*** |
15(12,0–17,0)*** |
12,0(11,0–14,0)*** |
11,0(8,0–12,0)** |
7,5(5,0–9,0)*** |
4,0(2,0–5,0)** |
|
CD25 |
17(15,9–18,1) |
15,5(13,0–17,0)*** |
13,0(10,0–14,0)*** |
10,0(9,0–12,0)** |
8,0(6,0–11,0)** |
5,0(3,0–7,0)*** |
3,0(2,0–5,0)* |
|
СD22 |
19,4(18,3–20,3) |
15,0(13,0–16,0)*** |
12,0 (10,0–14,0)** |
10,0 (8,0–12,0)*** |
8,0(6,0–9,0)** |
4,5(4,0–5,0)*** |
2,5 (2,0–3,0)*** |
Note — * p< 0.05, ** — p<0.01, *** — p<0.001; CG — Control Group
The amount of CD4 (T-helper) has also been reliably reduced in time intervals: 17–26 hours 30.5 % [25.35] (p<0.001), 27–36 hours 28 % [22.30] (p<0.05), 37–50 hours 23.5 % [20.27] (p<0.01), 51–64 hours [17.00 hours] (p after attack)<0.00–0.0.00].
Statistically significant decreases in CD8 (cytotoxic lymphocyte marker) were measured in time intervals of 7–16 hours 18 % to 27–36 hours 12 %, after 51–64 hours 7.5 % [17.19;12.17;11.14;5.9] (p<0.001), after 37–50 hours 11 % and 65–78 hours 4.17.17.17.11 % (p]<0.01] postmortem.
Decreases in receptor expression on T-lymphocytes to IL-2 (CD25) have been observed in time intervals: 7–16 hours 15.5 % to 17–26 hours 13 %, 51–64 hours 5 % [13.17.10.14.3.7] (p<0.001), 27–36 hours 10 %, 37–50 hours [9.12 %<0.01]and 65–78 hours after death 3 % [2;5] (p<0.05).
Decreases in CD22 receptor expression on B lymphocytes were noted in the following time intervals: 7–16 hours 15 % [13;16], 27–36 hours 10 % [8;12], 51–64 hours 4.5 % [4;5], 65–78 hours 2.3 % (p<0.001), 17–26 hours [12], 17–10 hours, and after 6 hours [0.5]
From the data presented, it appears that the amount of CD3-, CD4-, CD8-, CD25-lymphocytes are characterized by the highest correlation with the CSN and force of influence, which allows the use of these indicators in forensic practice (Table 2).
Table 2
The most statistically significant indices of T-lymphocytes expressing molecules CD3, CD4, CD8, CD25
|
Critical indicators |
Time of death |
|||
|
CD3 |
CD4 |
CD8 |
CD25 |
|
|
r |
-0,99 |
-0,99 |
-0,99 |
-0,99 |
|
p |
р<0,001 |
р<0,001 |
р<0,001 |
р<0,001 |
|
Force of influence |
99,87 % |
99,40 % |
99,57 % |
99,84 % |
|
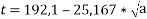
Regression Equation |
|
|
|
|
Note: t — TOD in hours; a — percentage of CD-positive cells
For CD3- and CD8-lymphocytes, the graph had a linear relationship, and for CD4- and CD25-lymphocyte, a regression dependence of the general form y=was used.
As a result of the analysis of the data, a reaction with anti-CD3 diagnostics is proposed to establish the TOD.
An example, of using the proposed method. The woman, 29 years old, died of multiple injuries. Tested the blood between 27 and 32 hours after death. The content of T-lymphocytes was determined, the expression molecule CD3–43 %. Using the formula, it was determined that 27 hours had elapsed since the time of death.
For the convenience of TOD determination, graphical dependencies of indicators of standard erythrocytic diagnostics — C3, CD4, CD8, CD22, CD25 derived by regression analysis can be used.
It has also been determined that the multiple injury assessment of nitrite/nitrate kinetics, reflecting nitrosative stress (Table 2), after 7–11 hours from the time of death, was 28 [27; 30], which was higher than the donor control group, 22 [20.5.28]. But 12–16 hours after death, the nitrate/nitrite level was lower at 16 [14;19] (p<0.01) and decreased to 5 [3;8] (p<0.001) after 17–21 hours.
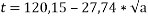
Because the NO molecule is short-lived and has not been studied postmortem, the task was given to study the change in the level of nitrate/nitrite in the plasma of the blood of corpses who died from Myocardial Ischemia and mechanical injuries depending on the TOD (Table 3).
When assessing nitrite/nitrate kinetics reflecting nitrosative stress, nitrite/nitrate levels were 61.5 (59.66) μmol/l after 2–6 hours in the first group of IBS deaths (n=17), much higher than the 22 (20.48.28.5) μmol/l control group. Further indicators decreased after 9–11 hours to 35 (31.38) μmol/l (p<0.01), and after 12–16 hours there was a sharp decline to 9 (6.12) /μmol/l (p<0.001).
Table 3
Dependence of the level of nitrate/nitrite in the plasma of the blood on the TOD of the deceased from MI and Mechanical injuries
|
cause of death |
Time since death (hours) |
|||
|
2–6 |
7–11 |
12–16 |
17–21 |
|
|
Myocardial Ischimia (n=17) |
61,5(59–66) |
35(31–38) ** |
9(6–12) *** |
- |
|
Mechanical injuries (n=11) |
- |
28(27–30) |
16(14–9)** |
5(3–8)*** |
|
Control Group (n=15) |
22 (20,48–28,5) μmol/l |
|||
Note — * — p< 0.05, ** — p<0.01, ***- p<0.001
In assessing the dynamics of nitrate/nitrite levels reflecting nitrosative stress, it was found that after 7–11 hours in the second group of deaths from mechanical injuries (n=11) the median (interquartile latitude) level of nitrate/nitrite was 28 (27.30) μmol/l. This was reliably higher than for the donor control group of 22 (20.5.28.5) μmol/l. But 12–16 hours after death, the level of nitrate/nitrite in the plasma was lower and amounted to 16 (14.19) μmol/l (p<0.01), and after 17–21 hours it decreased to 5 (3.8) μmol/l (p<0.001).
Analyzing the data obtained, it can be noted that in plasma of those who died from MI in the period from 2 to 6 hours after death there was a sharp increase in nitrate/nitrite levels. Then, starting from 7 hours after the death, this figure was reliably reduced and reached zero by the end of the day (Fig. 1).
Fig. 1. Dependence of blood plasma nitrate/nitrite level on TOD in deceased from MM and mechanical injuries
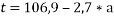
A regression analysis of the obtained data using the Statgraphics program was carried out. Taking nitrate/nitrite levels into account, the TOD can be determined by equation (1):
where t — TOD; a — the level of nitrate/nitrite in the blood plasma.
Construction was carried out in linear regression dependence. Correlation factor = -0.9996; p<0.001.
Here is an example. A 29-year-old woman died of blunt conjugate trauma when she fell from a height. Examined the blood about 12 hours after her death. Nitrate/nitrite levels of 16.25 μmol/L were determined. Using the plasma nitrate/nitrite ratio equation, we determine that 14 hours have elapsed since death.
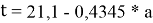
For ease of use, one of the graphs of the dependence of the level of nitrate/nitrite plasma on the TOD of the deceased as a result of MI and mechanical injuries can be used (Fig. 2).
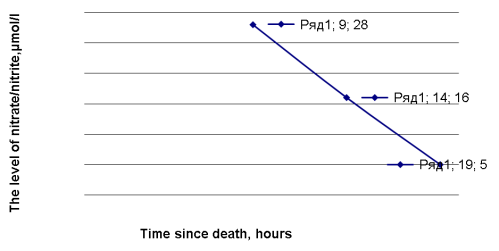
Fig. 2. Dependence of plasma nitrate/nitrite level on TOD in deceased due to mechanical injuries
Conclusion
- Number of deaths due to other causes of death
T- and B-lymphocytes expressing molecules CD3, CD4, CD8, CD22, CD25 are reliably reduced at all time intervals (up to 65–78 hours).
- In determining the most significant indicators for determining the TOD, there are significant differences in the phenotype of immune system cells (CD4-, CD8-, CD22-, CD25-cell) No one was identified, allowing any of these criteria to be used to determine the timing of the TOD.
- The number of CD3-, CD4-, CD8-, CD22-, CD25-cells is the most correlated with the TOD and the power of influence, which allows the use of methods to determine these values to estimate the TOD from and up to three days after death.
- Identification of CD receptors on lymphocytes by means of standard erythrocytic diagnostics with monoclonal antibodies makes it possible to determine the TOD by the content of the corresponding cells in standard conditions.
- The TOD can be established on the basis of a reliable reduction in the level of nitrate/nitrite in the plasma of deceased people — up to the first day from the time of death.
- Graphs and equations derived from regression analysis have been proposed for establishing the TOD and for practical use in forensic medicine, for changes in blood and nitrate/nitrite levels in plasma.
References:
- Melnikov Y. L., Zharov V. V. Forensic medical determination of time of death. M.: Medicine; 1978.
- Maiese A., Scatena A., Costantino A., et al. MicroRNAs as useful tools to estimate time since death. a systematic review of current literature // Diagnostics (Basel). 2021 Jan 3;11(1):64.
- Muggenthaler H., Hubig M., Schenkl S., Niederegger S., Mall G. Calibration and Parameter Variation Using a Finite Element Model for DeathTime Estimation: The Inuence of the Substrate. Legal Med., 25:23(28), 2017.
- Vacchiano G, Luna Maldonado A, Matas Ros M, Di Lorenzo P, Pieri M. The cholesterol levels in median nerve and post-mortem interval evaluation. Forensic Science International. 2016 Jan; 265: 29–33.
- Ortmann J, Doberentz E, Madea. Immunohistochemical methods as an aid in estimating the time since death. Forensicscienceinternational. 2017; 273: 71–9.
- Kazarnovskaya M. L. Blood lymphocytes in postmortem autolysis. Reproduction of corpse blood lymphocytes. Chisinau: Stiintza; 1983.
- Mishin M. Y. Special process of peroxidation oxidized in sudden death. Ukraine. court. -honey. vsn. 2007; 1(20):40–42.
- Kostylev V. I. Dependence of immune indicators of the blood of the deceased from diseases in the dynamics of the early postmortem period. Up. Theory and practice court. -medical. expertise. Zaporozhye; 1999: P. 76–77.
- Solaniai A. N. Possibility of forensic-medical determination of damage by changes of the enzyme NO-synthase in myocardium. Ukraine. morphol. alma. 2008; 11(4): 143–144.
- Anggard E. Nitric oxide: mediator, murderger, and medicine. The Lancet. 1994; 343 (14): 1199–1206.
- Golikov P. P. P., Nikolaeva N. Y., Gavrilenko I. A. Nitric oxide and lipid peroxidation as factors of endogenous intoxication in urgent states. Pat. physiology and experimentation. therapy. 2000; 2: 6–9.
- Sharshar T., Margentaler J. A., Landeros K. Apoptosis of neurons in cardiovascular autonomic centres triggered by inducible nitric oxide synthase after death from septic shock. The Lancet. 2003; 362 (9398): 1799–1805.
- Dwivedi Y., Rizavi H. S., Roberts R. C., Conley R. C., Tammings C. A., Pandey G. N. Рreduced activation an expression of ERK ½ MAP kinas in the post-mortem brain of depressed suicide subjects. Journal of Neurochemistry. 2001; 77 (3): 916–28.
- Novikov D. K., Novikov P. D., Yanchenko V. Y. Methods of determining T- and V-lymphocytes diagnostics based on monoclonal antibodies. Immunology, Allergy, Infectology. 2000; 2: 31–33.
- Solodkov A. P., Veremei I. S., Osochuk S. S., Shcherbinin I. Y., Deyun G. V., Dubrovskaya A. V. Photometric method of determination of nitrates and nitrites in biological liquids: instructions for use. Utv. M3 RB., 91–0008 from 19.03.2001.
- Rebrova O. Y. Statistical analysis of medical data. Application of STATISTICA. M.: Media Sphere; 2006.