In this review modern considerations about pecularities of imaging modalities used in pediatric practice are presented. The main patterns of the most common pathologies urinary tract are shown and methodical aspects of using conventional radiography, sonography are pointed out.
Keywords: radiography, ultrasound diagnostics.
Inflammatory diseases of the kidneys and urinary tract are one of the most common childhood diseases. Predisposing factors against which these changes most often develop can be various anatomical anomalies of the urinary system, for example, pathology of the ureter and pyelourethral segment, disrupting the normal excretory function of the kidney, changes in the vesicoureteral segment, leading to impaired urodynamics, changes in renal vessels that disrupt the blood supply to the kidney. These changes under the influence of an exogenous factor (hypothermia) contribute to the development of inflammatory changes in the parenchyma of the kidney and urinary tract.
The purpose of this study is determination of diagnostic tactics and sequence of application of various methods of radiation diagnostics in children with inflammatory diseases of the kidneys and urinary tract, comparison of the effectiveness of these methods in the diagnosis of various uronephrological pathologies .
Materials and methods. 176 children aged 2 to 14 years were examined, 52.8 % were girls, 47.2 % were boys. Ultrasound with color Doppler mapping (CDM) was performed on modern ultrasound (using a convex probe with a frequency range of 3.5–5 MHz) and X-ray machines (TITAN 2000, Korea).Ultrasound with CDC and excretory urography were performed in 56 (31.6 %) children; 22 (12.4 %) — ultrasound with CFD; in 20 (11.5 %) children, ultrasound with CDI was combined with excretory urography and ascending cystography; in 20 (11.5 %) children, ultrasound with CDI was performed with excretory urography; in 17 (9.6 %) — ultrasound with color doppler, excretory urography, ascending cystography; in 18 (10.3 %) patients, ultrasound with color doppler and ascending cystography were performed; in 18 (10.3 %) — only ultrasound with CFD; in 5 (2.8 %) patients — ultrasound with color doppler, ascending cystography.Of the 176 patients, 18 required only an ultrasound with CFD with the appointment of subsequent ultrasound dynamics. The remaining 158 patients after ultrasound with CDC required other radiation techniques. The following pathology was diagnosed: initial manifestations of inflammatory changes — in 133 children, a detailed picture of inflammatory changes in the kidneys and urinary tract — in 21 children, a «small» kidney — in 4 patients (hypoplastic in 3, wrinkled in 1). In addition, 8 patients had nephroptosis, 2 — pelvic dystopia of the kidney, 2 — rotation of the kidneys.Incomplete doubling of the cavitary system was diagnosed in 11 cases, complete — in 1 case. Cysts were identified in 3 children, calcification — in 1 child, angiolipoma — in 1 child. Froley's symptom on excretory urography was determined in 17 people, pathology of the ureter (stricture, high discharge, valve, kink) — in 8 children.Ultrasound with CDC made it possible to establish depletion of the vascular pattern in 25 patients against the background of a «small» kidney and a detailed picture of inflammatory changes; 9 had various vascular pathologies (the presence of an additional vessel, doubling, stenosis, bending of the renal artery). Arteriovenous malformation was diagnosed in 1 patient.
Results and discussion. The most popular way to diagnose and control vesicoureteral reflux is still considered ascending cystography, the main advantages of which are to obtain information about the details of the structure of the bladder and anatomy of the urethra, as well as the ability to classify vesicoureteral reflux in accordance with the Heikel-Parkkulainenb classification (1966), which is based on an assessment of the severity of throwing a radiopaque substance during ascending cystography.Vesicoureteral reflux is divided into active — occurs at the time of urination, i.e. at the time of detrusor contraction, and passive — when there is a constant free connection of the bladder with the contents of the ureter, there are also mixed forms of reflux (active-passive) (Fig. 1).

a) In the phase of maximum filling of the bladder, passive reflux

b) In the urination phase, active reflux
Fig. 1. Ascending cystography. Active-passive vesicoureteral reflux on the left, grade 4. Severe dilatation of the pelvicalyceal system, deformation of the calyces
However, a significant radiation exposure during ascending cystography, which is especially dangerous for girls, forces us to look for alternative approaches to the diagnosis of vesicoureteral reflux. In addition, the x-ray method cannot guarantee that vesicoureteral reflux, the manifestations of which in many cases are very limited in time (seconds), will certainly coincide with the moments of the images. Some of these alternative methods are ultrasound with color doppler and radionuclide cystography [2, 3, 5–8]. Ultrasound with CFD allows you to get an image of the movement of urine flows, evaluate the quantitative and qualitative characteristics of emissions that depend on the state of the transport function of the urinary tract.
Signs of vesicoureteral reflux on ultrasound with CDC are: dilatation of the ureter in the lower and upper sections with an average or maximum filling of the bladder and a stable expansion of the pelvis of more than 10 mm, regardless of the filling of the bladder (Fig. 2). If, after micturition, the pelvis has not decreased or even increased in size, then active reflux occurs, with a decrease in the size of the pelvis, passive reflux is diagnosed.

a) Echogram of the expansion of the cavitary system of the kidney

b) Echogram of the dilated ureter
Fig. 2. Echograms on the background of the bladder: 1 — bladder, 2 — ureter
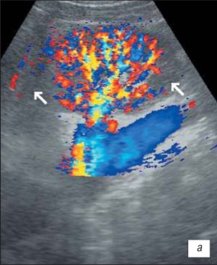
In addition, in the presence of vesicoureteral reflux, ultrasound with CDC can determine: a decrease in the size of the kidney on the side of the lesion; cyclic change in the diameter of the ureter in the upper and (or) lower sections; dopplerographic registration of the reverse flow of urine in the ureter in the form of a single-humped curve with a decrease in all quantitative indicators; the vertical orientation of the ureterovesical ejection, which normally has a direction at an angle of 30–40° relative to the imaginary line connecting the orifices of the ureters (Fig. 3).
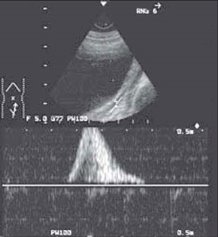
Fig. 3. Vesicoureteral reflux with ultrasound in the CFM mode
Scanning of the ureter through the bladder.
Flow velocity 11 cm/s (norm up to 20.3 cm/s), flow time 1.16 s (norm 6.2 s).
It should be noted that changes in the kidneys and urinary tract, which are detected by ultrasound with CDI and dynamic angionephroscintigraphy, are not specific for a particular disease, but characterize structural changes and impaired functional abilities of the urinary system. Diagnoses of pyelonephritis or glomerulonephritis are, in our opinion, primarily clinical, they can only be made with a combination of syndromes: clinical picture, physical examination data, changes in analyzes and, of course, changes that are determined by radiation diagnostic methods.
Ultrasound makes it possible to detect changes in the grey-scale mode, and, in combination with color flow, to characterize in detail the blood flow in certain parts of the vascular bed of the kidney and to establish, if any, vascular pathology [2, 4–6].
In the initial period of inflammatory changes, ultrasound with CDI reveals moderately pronounced diffuse changes in the parenchyma of the kidney against the background of maintaining the clarity of cortico-medullary differentiation (CMD); the contours of the kidneys are preserved, clear, even; unexpressed dilatation of the pelvis (without thinning of the parenchyma); intrarenal vascular pattern of the kidney preserved; speed indicators of arterial renal blood flow remain within the normal range.
With a detailed picture of ultrasound with CDI, it is characterized by unevenness, fuzziness, deformation of the kidney contour, which in some places may not be traced; the kidney is sometimes poorly differentiated from the surrounding tissues in places, which makes it difficult to determine its size; small, irregularly shaped retractions of the contour are visualized, distributed either along the entire contour, or in some fragment of the kidney; fuzziness of cortico-medullary differentiation is determined;
there are pronounced diffuse changes in the parenchyma of the kidney with a moderate uneven increase in its echogenicity; dilatation of the pyelocaliceal system; fragmentary thinning of the kidney parenchyma with compensatory thickening or preservation of the thickness of its other parts (Fig. 4); moderate depletion of the intrarenal vascular pattern, most pronounced in places of deformation and retraction of the kidney contour; decrease in the speed characteristics of arterial blood flow (Fig. 5).
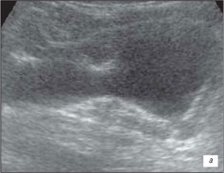
a) Inflammatory changes in the kidney

b) Retraction on the contour of the kidney (arrow)
Fig. 4. Echogram of the kidney
a) Intrarenal vascular pattern of the kidney is preserved, cortical blood flow is determined in all parts of the parenchyma

b) Depletion of the vascular pattern
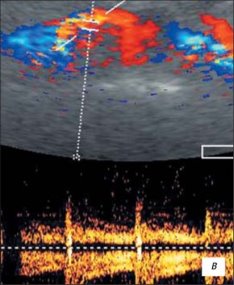
c) Velocity indicators at the mouth of the renal artery within the age norm: Vps — 83.7 cm/s; Ved — 34.1 cm/s; RI — 0.63; PI — 0.96
Fig. 5. Ultrasound of the kidney with inflammatory changes in the color flow mode
Ultrasound with CDK reveals anomalies in the number, position and structure of the kidneys; diffuse and focal changes in the parenchyma. The method is highly sensitive to urinary tract obstruction. In addition, he orients regarding the nature of the disease and determines the choice of a further imaging method.
Ultrasound with CDC has advantages over excretory urography in severe hydronephrosis. Significant dilatation of the pyelocaliceal system leads to a strong «breeding» of the contrast agent and the pyelocaliceal system of the kidney on the excretory urogram may not be contrasted, which causes the diagnosis of a «non-functioning» kidney. Conducting ultrasound on high-resolution devices with an assessment of renal blood flow avoids this error.
Preservation of normal echogenicity of the parenchyma even against the background of its thinning to 3–4 mm and a sharp dilatation of the pyelocaliceal system, provided that the vascular pattern of the kidney is visualized at least only in the projection of the pelvicalyceal system and the medullary layer, and a decrease in the average blood flow velocity by no more than 2 times when compared with the collateral kidney is prognostically favorable [4].
However, ultrasound with CDC has disadvantages: it does not always allow visualization of the ureters and does not provide complete information about the function of the kidneys. Therefore, it is recommended to perform radionuclide studies and (or) excretory urogram after performing ultrasound with CFD, depending on clinical indications, and only if necessary, perform ascending cystography.
An excretory urogram provides an overview of the entire urinary tract, including the ureters and bladder; allows you to evaluate the excretory function of the kidneys; confirms or excludes obstruction, determines the causes and level of obstruction.
The specified approach in diagnostics and adherence to a strict sequence of performing radiation techniques makes it possible to diagnose vesicoureteral reflux (ultrasound with CFD), evaluate kidney function (excretory urography), determine the pathology of blood vessels (ultrasound with CFD), ureter and bladder (excretory urography).
The combination of ultrasound with CDI and ascending cystography is not effective enough. Given the low percentage of detection of refluxes in ascending cystography, as well as various diffuse and structural changes in the kidneys detected during ultrasound with CFD, we cannot fully determine the function of the kidneys, changes in the ureter, and therefore, confirm or refute the changes detected by ultrasound.
Conclusion. The combined use of ultrasound with CDC and radiographic methods of investigation to detect vesicoureteral reflux makes it possible to exclude ascending cystography in many patients. The first imaging modality in children with kidney and urinary tract pathology should be CFD ultrasound. X-ray diagnostic methods should be used strictly according to indications.